“The secret of change is to focus all of your energy, not on fighting the old, but on building the new.” – Socrates
Socrates, an Ancient Greek philosopher, was widely considered one of the three most influential philosophers, along with Plato and Aristotle, in Ancient Western philosophy. And based on a study of his life and musings, it is easy to understand why his statements are still relevant today, especially in the Post-COVID-19 era.
Without going into the background of “everything SARS-CoV-2,” it is worth noting that this virus is here to stay, at least for the foreseeable future. This quotation provides the quintessential attitude that the world’s citizens need to cultivate in order to face the challenges of living with the novel coronavirus.
Therefore, the question that must be asked and answered is how do we, the citizens of the world, join together with medical professionals, research scientists, and national and federal governments to find a solution to the extremely contagious novel coronavirus?
The straightforward answer to this question is to donate blood for research if you are a COVID-19 survivor.
COVID-19 convalescent plasma: A description and brief history
Before we look at current research studies and efforts to determine whether convalescent plasma is a viable treatment regime for COVID-19 sufferers, let’s take a step back and have a look at what convalescent plasma is and a brief history of its uses as an antiviral treatment.
What is convalescent plasma?
In order to understand the phrase “convalescent plasma,” let’s divide it up into two sub phrases and look at the meaning of each individually:
- Convalescent
The term “convalescent” refers to anyone who is recovering or has recovered from an illness or disease. In the COVID-19 context, it represents individuals who have recovered, or who are recovering, from the illness caused by the SARS-CoV-2 virus.
- Plasma
Plasma is a component of whole blood. The urmc.rochester.edu website defined plasma as the often-forgotten part of blood. It is a vital element of whole blood, along with red blood cells, white blood cells, and platelets. Succinctly stated, it is the yellow fluid that carries the other blood components throughout the body.
Convalescent plasma contains antibodies, or immunoglobulins, a protective protein produced by the immune system in response to a foreign object like a virus or an infection, called an antigen. Antibodies attach themselves to these antigens to notify the immune system that the virus is a foreign body and must be destroyed by the body.
A brief history of the successful use of convalescent plasma
Convalescent plasma is a reasonably old treatment that has been around for over 100 years. The journal article titled “The true historical origin of convalescent plasma therapy” describes convalescent plasma as a passive immunization strategy first used during the Spanish Flu pandemic.
This article also notes that several studies conducted during the Spanish Flu pandemic suggested that convalescent plasma could be effective in reducing the risk of mortality when infected with the virus.
Convalescent plasma has subsequently been used as a treatment regime in the SARS-CoV-2, MERS, West Nile virus, and Ebola virus outbreaks. While the evidence cannot be considered 100% successful because no double-blind placebo studies have been conducted, there is substantial evidence that demonstrates that, if administered early after the onset of the symptoms, there is a marked reduction in the fatality rate.
The only caveat here is that Ebola sufferers treated with convalescent plasma showed very little to zero improvement. However, it was measurably successful in both the SARS and MERS epidemics.
Fast forward to 2020 and the SARS-CoV-2 pandemic
The FDA issued an Emergency Use Authorization for convalescent plasma as a promising COVID-19 treatment on 23 August 2020.
This decision was based on the results of studies conducted by organizations such as the Mayo Clinic. The Mayo Clinic study enrolled over 35 000 patients and gave each patient antibody-rich convalescent plasma at different stages of their illness. The following outcomes were noted:
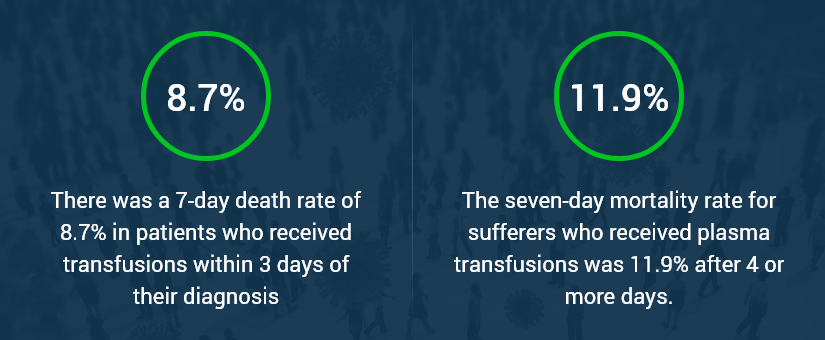
- There was a 7-day death rate of 8.7% in patients who received transfusions within 3 days of their diagnosis.
- The seven-day mortality rate for sufferers who received plasma transfusions was 11.9% after 4 or more days.
In summary, “the difference met the standard for statistical significance.”
Challenges faced by doctors and researchers
Although there are to date over 27 million infected people across the globe, the pool of individuals who are in a position to donate blood is quite small. Statistically speaking, there are 7.594 billion people who live on planet earth. 27 million people is only 0.36% of the global population.
There are several caveats to this calculation:
- This statistic is solely designed to highlight that the available pool of possible convalescent plasma is tiny; thereby, presenting a challenge to global healthcare professionals if this treatment is approved as part of the mainstream treatment regime.
- 27 million infected people as individuals is a catastrophic number of infections, and not only has it brought many national healthcare systems to their knees; these people are all beloved family members and should not have had to die.
- This virus is extremely contagious and spread via person-to-person contact, consequently, these numbers change daily.
Secondly, there is a valid concern that the success rates of the convalescent plasma are skewed for the following three reasons:
- Double-blind and randomized placebo trials have not yet been conducted. A few of these trails have just started. The C3PO, short for Clinical Trial of COVID-19 Convalescent Plasma of Outpatients, run at several Michigan hospitals focuses on treating sufferers with the plasma as soon as they arrive at one of the participating hospitals’ outpatient departments. Not every patient will receive the convalescent plasma. This is a randomized trial, with 50% of patients receiving a saline placebo.
- Every bag of frozen human convalescent plasma is not equal. Some bags will contain a more significant number of antibodies, while others will have fewer antibodies. As a result, this scientific variable cannot be excluded to produce an exact result.
- Research scientists know very little about the SARS-CoV-2 virus’s behavior. Moreover, according to Harlan Krumholz, director of the Center for Outcomes Research and Evaluation at Yale New Haven Hospital, “it raises the question of what strength of evidence is necessary to treat during a pandemic…The problem is we have yet to resolve what is sufficient evidence to change the treatment paradigm.”
Final thoughts
Finally, there is an urgent need for blood donors who have recovered from COVID-19 and can provide research laboratories like ours with a blood donation for convalescent plasma, especially now that the FDA has authorized convalescent plasma as an emergency treatment for COVID-19.
Note: at Solomon Park Research Labs, we use your blood donations to create in vitro COVID-19 convalescent plasma samples to research studies and medical labs as part of the global effort to understand the virus’s behavior to find a successful treatment regime to prevent the loss of life, control its rampant spread, and to find a vaccine that will protect the majority of the global citizens.
Partner with us to help the world fight the global pandemic caused by the SARS-CoV-2 virus.